
Surgery
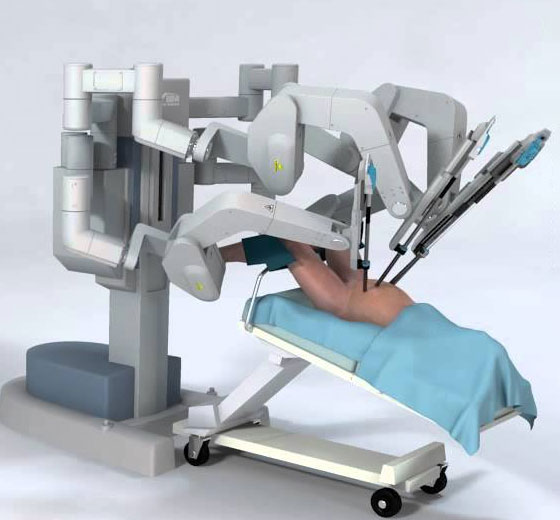
Robotic Radical Prostatectomy
Robotic Radical Prostatectomy is a minimally invasive robotic surgery in Kerala used for Prostate Cancer Treatment . During the procedure, a surgeon uses a robotic system to remove the entire prostate gland and surrounding tissue.
- Minimally invasive
- Robotic precision
- 3D visualization
- Reduced pain
- Low risk of recurrence
Surgery
Robotic Radical Nephrectomy
Robotic radical nephrectomy is a robotic surgical procedure that involves the removal of a kidney, along with the surrounding tissues and lymph nodes, using a robotic system.
- High precision
- Enhanced visualization
- Reduced complications
- Faster recovery
- Preservation of kidney function


Surgery
Robotic Partial Nephrectomy
Robotic Partial Nephrectomy is a minimally invasive robotic surgery used to remove a portion of the kidney affected by a tumor or other abnormal growth.
- Careful removal of kidney tumors
- Radical Cystectomy with Orthotopic Neobladder
- Faster recovery time than normal open surgery
- High success rate
Surgery
Robotic Pyeloplasty
Robotic pyeloplasty is a minimally invasive robotic surgery that is used to treat a condition called ureteropelvic junction obstruction (UPJO).
- Robotic system
- Safe and effective treatment
- Improved outcomes
- Faster recovery


Surgery
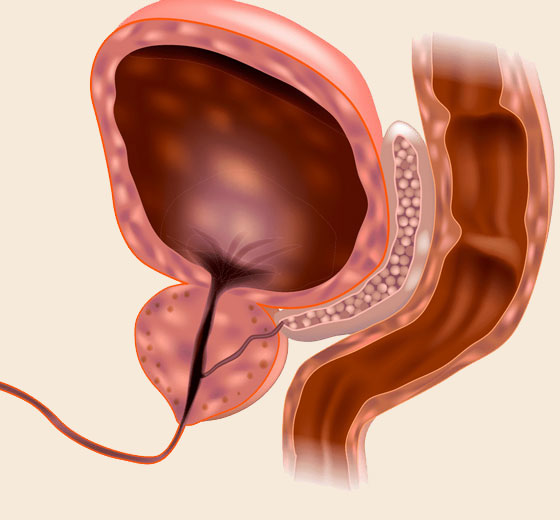
HoLEP (Holmium Laser Enucleation of the Prostate)
HoLEP involves enucleation of the prostate rather than resection to achieve a near-total removal of the prostate gland.
- No risk of TURP syndrome
- Maximum gland removal
- Least recurrence risk
- Better Urinary flow
Surgery
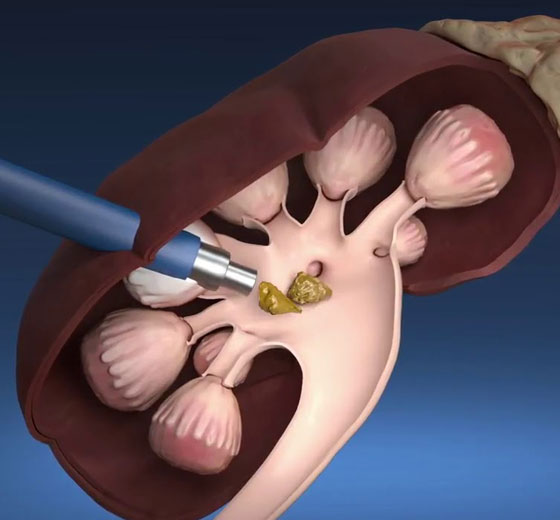
Retrograde Intrarenal (RIRS)
Retrograde Intra Renal Surgery (RIRS) is a minimally invasive surgical procedure used to treat kidney stones and other conditions affecting the urinary tract.
- Laser stone fragmentation
- Minimally invasive surgery
- Flexible ureteroscope
- Kidney stone removal
- Non-surgical treatment option

Surgery
Mini PCNL
Mini PCNL stands for Mini Percutaneous Nephrolithotomy, which is a minimally invasive surgical procedure used to remove kidney stones.
- Nephroscope-guided stone removal
- Small incision kidney stone surgery
- Modified PCNL procedure
- Precision stone removal surgery
Surgery
Urethroplasty
Urethroplasty is a surgical procedure used to treat urethral strictures, which are narrowings or blockages in the urethra, the tube that carries urine from the bladder out of the body.
- Urethral reconstruction
- Tissue grafting
- Penile surgery
- Urinary blockage treatment
Surgery
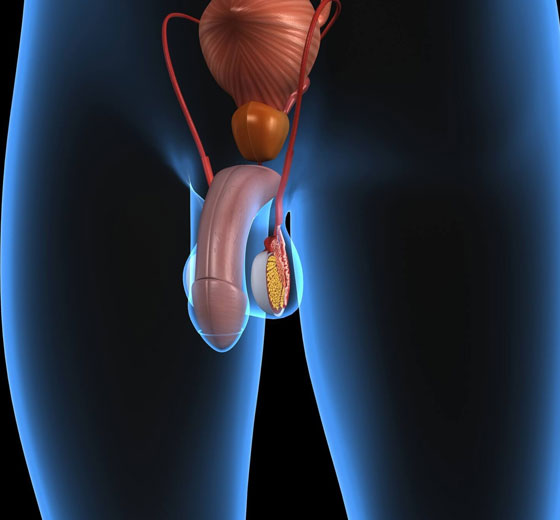
Penile Prosthesis Procedure
Penile Prosthesis Procedure is a surgical procedure used to treat erectile dysfunction (ED) in men who have not responded to other treatments such as medication or vacuum erection devices.
- Implantable Penile Device
- Erectile Dysfunction Treatment
- Surgical ED Treatment
- Prosthetic Penis Implant
Surgery
Microscopic Subinguinal Varicocelectomy
Microscopic sub-inguinal varicocelectomy is a surgical procedure that is used to treat varicoceles, which are enlarged veins in the scrotum that can cause pain, discomfort, and infertility.
- Fertility restoration
- Minimally invasive
- Microscopic approach
- Regional anesthesia
- Low recurrence rate
- Small incision


Treatment
UroLift
The UroLift system is a simple procedure that uses small implants to lift and hold enlarged prostate tissue, allowing for unobstructed urine flow. It does not involve cutting, heating, or removing any prostate tissue.
- One-Time Solution
- Faster Recovery
- Improved Urine Flow
- Rapid Relief
- Straightforward Procedure
FAQ
The procedure is generally carried out by a robot, which consists of small tools attached to a robotic arm that is controlled by a computer. One of the most widely used robotic systems in the world is the “Da Vinci system”.
- Prostate cancer
- Kidney cancer
- Kidney blockage
- Reconstruction of the kidney, ureter, and bladder
- BPH prostate removal
- High level of precision
- Flexibility
- Saves time
- Reduce manual labor
- Effective surgery in difficult-to-reach areas
- Increased recovery time
- Infection risk is low
- Scars are less





